-
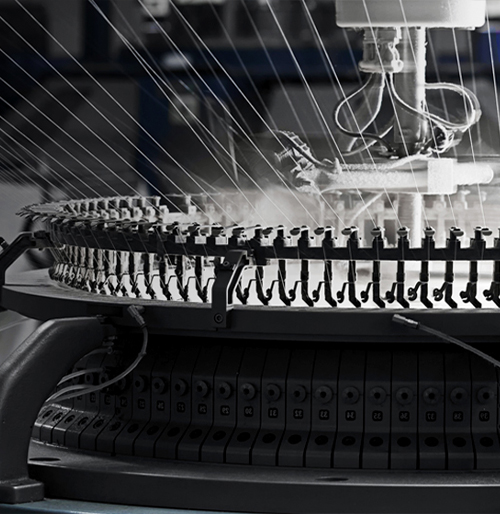
 General Purpose Gloves - CoatedMaxiFlex® Ultimate™34-874
General Purpose Gloves - CoatedMaxiFlex® Ultimate™34-874
-
 Cut Resistant GlovesMaxiFlex® Cut™34-8743
Cut Resistant GlovesMaxiFlex® Cut™34-8743
-
 Safety HelmetsTraverse™280-HP1491RVM
Safety HelmetsTraverse™280-HP1491RVM
-
 Hi Performance GloveBoss®9916
Hi Performance GloveBoss®9916
-
 Cut Resistant GlovesMaxiCut® Ultra™44-3745
Cut Resistant GlovesMaxiCut® Ultra™44-3745
-
 Hi Performance GloveG-Tek® PolyKor®16-MPT630
Hi Performance GloveG-Tek® PolyKor®16-MPT630
-
 Extended Use Disposable GlovesGrippaz™ Skins67-246
Extended Use Disposable GlovesGrippaz™ Skins67-246
-
 Extended Use Disposable GlovesGrippaz™ Engage67-307
Extended Use Disposable GlovesGrippaz™ Engage67-307
-
 Arc Protection KitsPIP®9150-52436
Arc Protection KitsPIP®9150-52436
-
 Safety HelmetsKilimanjaro™280-HP642R-CH
Safety HelmetsKilimanjaro™280-HP642R-CH
-
 Hi Performance GloveG-Tek®120-5150
Hi Performance GloveG-Tek®120-5150
-
 Safety HelmetsKilimanjaro™280-HP642RV-CH
Safety HelmetsKilimanjaro™280-HP642RV-CH



















 (3).jpg)